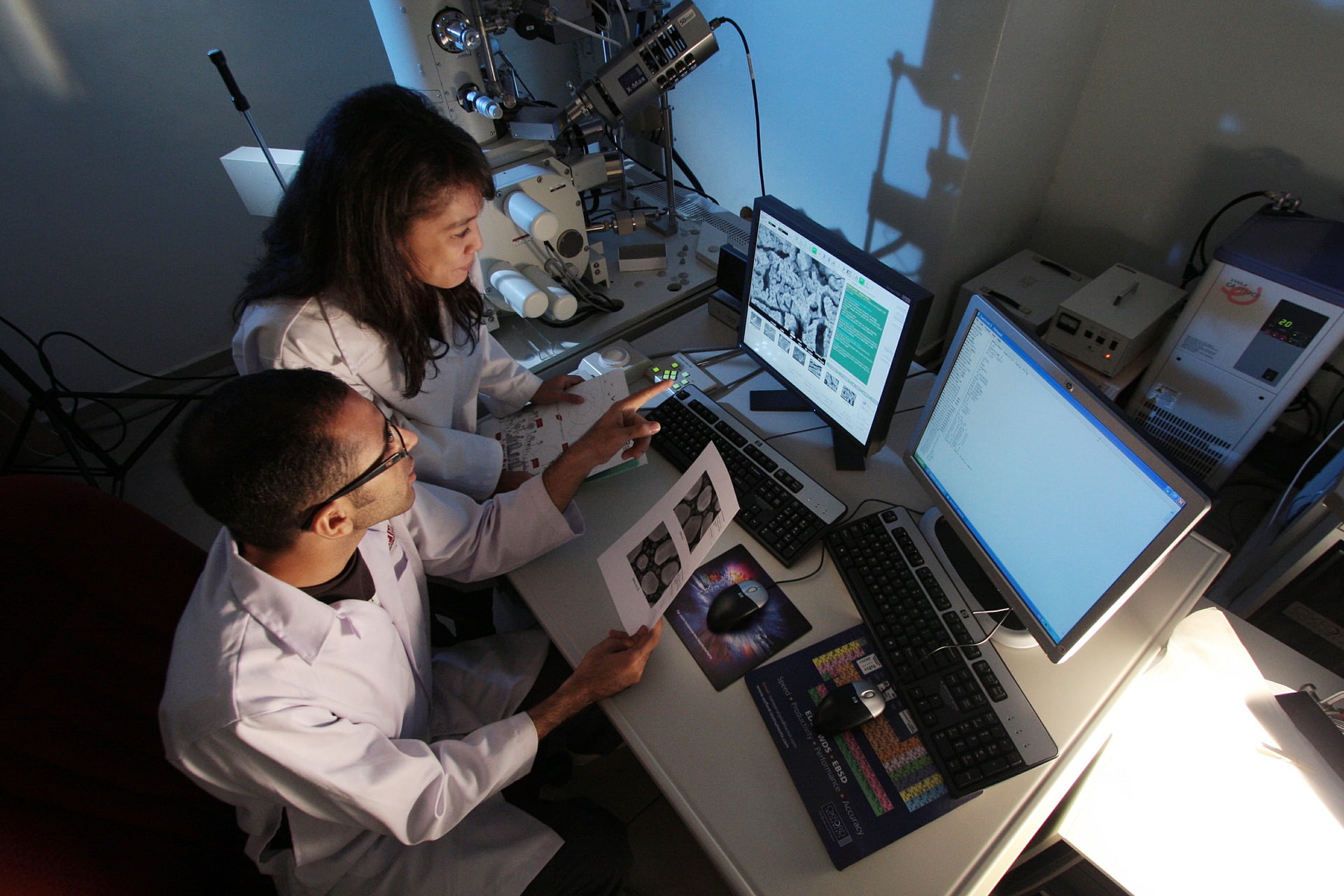
At the Rocky Mountain MS Center, we know that clinical research is critical to understanding this disease’s complex triggers and effects, and will lead to better treatments and ultimately the cure.
The Rocky Mountain MS Center at University of Colorado is the home of one of the largest MS research programs in the world. The success of our clinical research programs depends on the broad support of the MS community in the Rocky Mountain MS Center region. Together we are stronger than MS.